More often than not when one is defiled or raped they become helpless. Life suddenly becomes unbearable and the thought of seeking justice is far-fetched. This happens because survivors suffer stigma. It should not be the case, one needs to report and legal action taken to stop these heinous acts. You could be wondering how to I go about this, well here is how.
In case of Rape
• Don’t take a bath. Even though it is a natural reaction to want to wash, do not take a shower or bath as this may destroy vital evidence needed in your case.
• Do not change your clothes as these may carry blood, semen and other bodily fluid which can be used as evidence. If you have to change clothes, DO NOT keep clothes in a PLASTIC BAG.
• If you can manage, do not go to the toilet or brush your teeth.
• Don’t drink any alcohol or take any medication before going to the police since this can influence the outcome of the medical examination, and you will also need to make a statement.
• Contact a friend/family member you trust for support. The first person you tell about the rape is called the first witness. This person may need to make a statement to the police about your condition and if possible, should accompany you to the hospital/police station.
• See a doctor first
• It is recommended that you visit the nearest clinic, hospital or doctor first. It is preferable to not visit a family doctor as he/she may not be trained for this type of medical investigation. The doctor must be willing to testify in court.
• Report to a police station and record a statement. Make sure you take the OB number.
Dealing with the police
Initially only a brief statement is required from you. Make sure you read over the statement before signing it. You can provide a more detailed statement later.
You must get the P3 Form. The Kenya Police Medical Examination form, popularly known as P3, is provided free of charge at our police stations. It is used to request for medical examination from a Medical Officer of Health, in order to determine the nature and extent of bodily injury sustained by a complainant(s) in assault cases. Part I of the form must be filled by the Police Officer requesting medical examination.
Part II must be filled by a Medical Officer or Practitioner carrying out the examination giving medical details. This form is a government document and must be returned to the police for use in adducing evidence in court. Once the P3 form is filled in at the police station, the complainant is escorted by a police officer to a medical officer or practitioner for examination. The form becomes an exhibit once produced in court.
At the police station you have the right to:
• Make your statement in a private room
• Make your statement to a female officer (if there is one)
• Make your statement in your own language
• Have a friend/family member with you for support
• Get a copy of your affidavit (you are entitled by law), name of the investigating officer and case number.
• Get the OB number of the police station you can call to check progress on your case.
• If a suspect has been caught, make sure they inform you of a bail application. You have no right to testify at the bail application, but you can find out the name of the prosecutor and the court where the hearing will take place.
• You can approach the Chief Prosecutor or Prosecutor in charge of Sexual Offences before the bail hearing and disclose your fears if the suspect is released on bail.
What happens during the medical examination?
Try and remember. Provide as much details as you can of the incident to the doctor examining you. This may serve as useful evidence.
Rape kit
The doctor needs to complete a rape kit, this includes taking note of any injuries, scrapings under finger nails, evidence of sperm from your vagina and looking for possible DNA.
No male officer may be present at the examination and once again, you have the right to have a friend or relative with you to support you.
HIV
It is important to get PEP within 72 hours of penetration, attempted penetration, oral sex, or anal sex to reduce the possibility of contracting HIV.
Before getting the medication, you will need to undergo an HIV test.
STDs and pregnancy
During the first doctor’s examination you may need to take in quite a lot of medication. Doctors may prescribe medicines to prevent sexually transmitted diseases and further infections such as hepatitis, and to prevent pregnancy.
If you are already pregnant when you are raped, talk to the doctor about the possibilities of your unborn baby becoming infected with HIV.
Forensic evidence
Doctors may ask for your clothes and other evidence which will be sealed in a paper, not plastic bag. Plastic bags can cause degradation of biological material (such as semen) as a result of the heat in the bag.
All evidence is entered into a special police crime kit.
Getting support
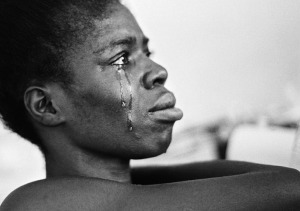
Rape Trauma Syndrome (RTS) is a form of Post-Traumatic Stress Disorder (PTSD) that often affects rape survivors. This psychological disorder can be very debilitating. It is important to get some form of support or counselling after being raped, as you will have many emotions and concerns that you will need to work through.
If you are in Kisumu you can visit Gender Violence Recovery Centre at Jaramogi Oginga Odinga Teaching and Referral Hospital (Russia)
Call us for free on 0800724500 or contact these numbers for help; Child line Kenya-116 and Health Assistance Kenya-1195.
Help us break the silence on such instances of human rights violation by sharing your story with us. It is through the documented cases that we can demonstrate how real the situation is and influence programs to support survivors